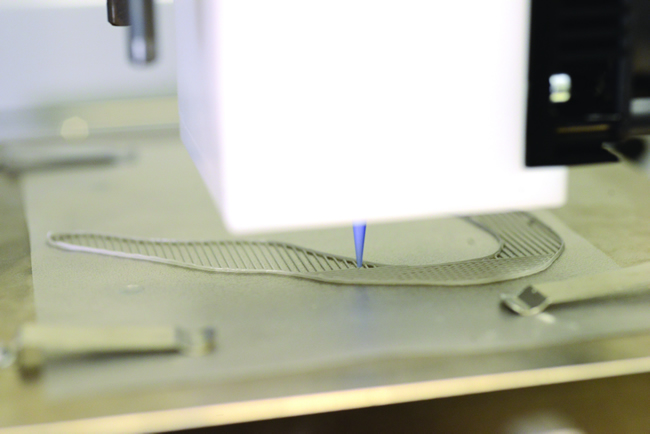
A 100-micron thick filament of silicone flows from the printer's nozzle.
The Next Generation of 3D Printing
UTSA acquires biomedical engineering device that can 3D print organs
The Department of Biomedical Engineering at The University of Texas at San Antonio has acquired a rare piece of equipment that can print organic tissues and potentially regenerate organs. The device works similarly to a 3D printer and is now a part of the laboratory belonging to Teja Guda, assistant professor of biomedical engineering.
"There aren't very many organ printers of this caliber in the world owned by universities," Guda said. "We wanted to explore this new space in regenerative medicine since so many at UTSA have strengths in regenerative medicine."
The aspect that sets this device apart from other 3D printers is that it is capable of printing live cells without killing them. In a traditional 3D printer, the ink is pushed through a nozzle using heat or high pressure, but Guda's printer doesn't use either of those mechanisms. And though the printing device itself is rare and costly, Guda and his students' real research focus is on the inks that will be developed to run through the device.
"Essentially, we're creating our own materials with embedded living cells," Guda said. "We load them up in little syringes, insert them into the machine, and it prints the organ layer by layer. Unlike traditional manufacturing techniques, it allows for very thin, complex architectures. The ink is the truly novel part of our research."
Guda and his team of graduate students have begun testing the printer with silicone to measure its geometric accuracy and see how the technology works so they know what properties will allow them to print with a good enough resolution with living cells. The team soon hopes to move into printing grafts for bones, skeletal muscle, pancreas tissue, and salivary glands.
"Bone and muscle are where we are going to get started," said Guda. "We have a lot of experience working with them and are more familiar with these tissues at this point. Plus, their makeup is much simpler. The number of cell types are far fewer."
Guda said that theoretically, a printer like the one in his lab could be inside an operating room and be filled with the patient's own cells. Then, the needed tissue would be printed right there in the operating room within a few hours and implanted in the patient. But as of right now, the research is just kicking off.
"The technology in terms of the inks doesn't exist right now," said Guda. "But we are getting those building blocks in place right here at UTSA."
Because the organs are printed from a gel of living cells, the challenge is to make sure the organ keeps its shape and the cells stay alive once it's been printed. The device is also expected to support research into the complications of organ transplantation, including tissue compatibility and survival.
"Transplantation of tissues is a huge challenge because they're not always successful and they're limited in supply," Guda said. "If we're able to make transplantation significantly more successful, that's huge."
The printer might also help engineers print a replacement for a person's damaged organs, which Guda predicts will be possible in less than 10 years.
"This is a building block for the future," he said. "Our students will benefit greatly from having this experience. As a university, we've gotten in on the ground floor."










