Engineering Professor Creates New Laser Needle
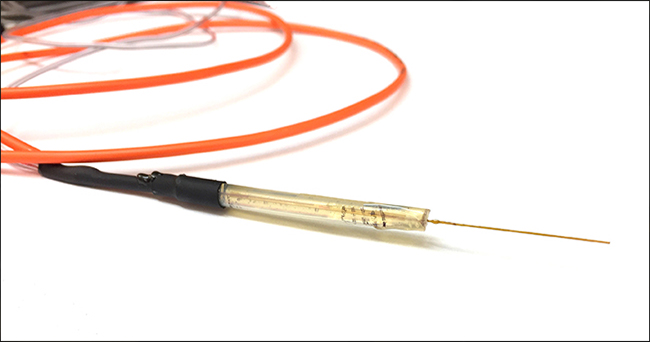
Lyle Hood, assistant professor of mechanical engineering at UTSA, has collaborated with Christopher Rylander, associate professor of mechanical engineering at The University of Texas at Austin, to create a device that can do the work of both a cutting-edge surgical needle and a medical laser.
The device has innumerable applications, most notably the ability to eradicate cancerous tumors while also delivering chemotherapy drugs.
Hood originally developed the needle to treat transitional cell carcinoma, which forms on the interior of the bladder.
“Treating cancer in the bladder is difficult if you want to preserve the organ’s ability to hold fluid,” he said. “The most typical treatment is to remove the bladder altogether, leaving patients with the need for a urinary bag for the rest of their lives.”
To solve this challenge, Hood and Rylander created the laser needle with Mehmet Kosoglu, then a graduate student at Virginia Tech. The needle penetrates the tissue to deliver medicine while emitting laser light that kills the tumors without making a hole in the bladder.
He soon discovered that his creation could treat other forms of cancer, including brain cancer, which is challenging to treat.
“The problem is that typical chemotherapy for brain cancer involves an IV in the arm, but due to the blood-brain barrier, not enough of that concentrated medicine enters the central nervous system and reaches the tumors,” Hood said.
Another brain cancer treatment involves dripping chemotherapy into the brain through a catheter inserted through the skull. However, because the brain is a closed fluid environment, too much medicine too quickly can cause overpressure, causing more harm than the tumor itself. As a result, not enough medicine reaches the cancer during this treatment. By using the laser needle to slowly heat the tissue during the drip, the chemotherapeutics will disperse much more rapidly and widely.
“I didn’t want patients sitting with a catheter in their head for three days, but they obviously need enough chemotherapy to kill the tumor,” Hood said. “This solves both problems.”
Hood noted that his device can even work in cosmetic surgeries; the laser can melt fat and the needle can remove it.
“If you melt the fat in place, the body just reabsorbs it, resulting in high levels in the blood,” he said. “This is why many existing laser treatments are not very healthy.”
For now, Hood is focusing on how his needle can be used to treat other types of cancer, particularly skin cancer.
“The idea is to take the creative approach,” he said. “We can go straight in and treat the problem locally without having to circulate chemotherapy.”
By Joanna Carver/University Communications and Marketing